From Gut-Wrenching Illness to a Poop Transplant that Saved My Life

In 2007, I was in the fight of my life—one that reshaped everything I thought I knew about health, medicine, and the incredible power of the microbiome. It all began with a bout of Campylobacter jejuni food poisoning. I was hospitalized with infectious colitis, facing relentless gastrointestinal distress, dehydration, and overwhelming fatigue. Yet, the nightmare was far from over.
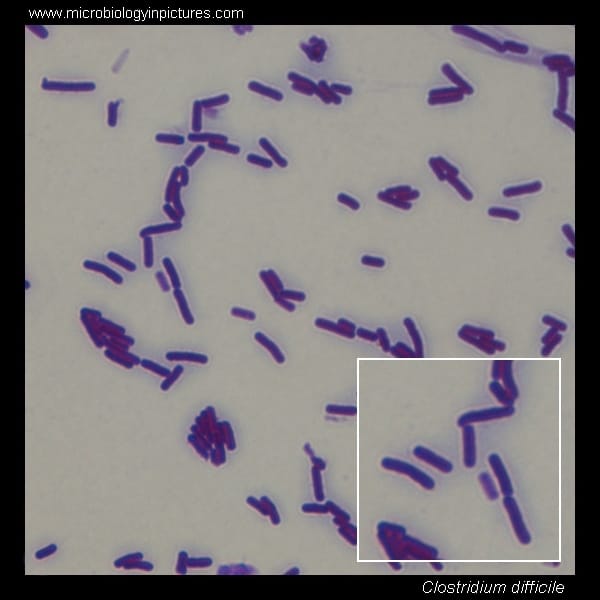
Despite being on high-dose antibiotics, I contracted a resistant Clostridioides difficile (C Difficile) infection—likely through lapses in hospital hygiene. The result? I was trapped in a cycle of fever, intense cramps, and diarrhea—up to 30 bathroom trips a day. Over months, I lost 30 pounds, felt weak and floated between hospital stays on IV vancomycin and other potent antibiotics. Every time the treatment stopped, my temperature spiked to 102°F, the symptoms returned, and I felt like I was dying.
Hearing the “Ick” Factor—and Finding Hope
At the lowest point, reliant on painkillers and more rounds of antibiotics with no reprieve, I watched a report on The National by Peter Mansbridge. He highlighted the challenge Canadian doctors faced in overcoming the "ick" factor—and introduced Dr. Thomas Louie and his pioneering work on fecal transplants at Calgary’s Foothills Hospital. Impulsively, I emailed Dr. Louie that night, and soon I was booked on a flight to Calgary.
In the midst of it all, a household joke emerged:
“Don’t go looking for ice cream in the Häagen-Dazs container in the basement—you won’t find what you think!”
We clung to humour because it was all we had.
A Journey Through Isolation—and Healing
On that flight, I was highly contagious and I spent most of the trip in the airplane lavatory—logging 20+ bathroom visits at 30,000 feet. When I landed and had my transplant procedure, I returned home just two days later, and for the first time in months, used the bathroom just once. It was miraculous.
Behind the Scenes: The Donor Process
As a mom, it was touching—and deeply agonizing—to see my young 12 year old son at the time go through the rigorous donor screening just so I could have a chance to get well. It was also beneficial that he was a blood relative, which increases the likelihood of microbiome compatibility.
Step-by-Step: How Feces Is Prepared for Fecal Transplant
- Donor Screening (My Son)
- Blood work and lab tests (HIV, hepatitis, Salmonella, E. coli, parasites, antibiotic-resistant organisms)
- Assessments for chronic GI issues (IBD) and autoimmune disorders
- Only about 3–10% of volunteers qualify—the process was exhaustive and nerve-wracking for us both.
- Stool Collection
- A fresh sample was collected over a couple of days.
- Collected in a container, following medical protocol
- Processing the Stool
- In a sterile lab at the hospital in Calgary, the sample was mixed with saline (sometimes with glycerol)
- Blended and filtered to remove debris
- Result: a homogenized microbial suspension packed with beneficial bacteria
- Delivery
- My case was handled via a fecal enema, administered in a private apartment next to Calgary's Foothills Hospital
- The enema bag was hung from a dresser—a surreal science-powered moment of hope
Why FMT Works for C. difficile:
C. difficile infections often follow antibiotic use, which disrupts the natural gut microbiome. FMT restores a healthy bacterial balance, outcompeting C. difficile and allowing the gut to recover.
The Transplanted to Transformation
After that infusion, the transformation was swift. Within two days, bathroom visits plummeted from dozens to just one. I was thin, nutrient-depleted, and weakened by illness—but my gut had been rebooted. Over the following months, I rebuilt my microbiome, nutrient stores, and resumed living—and thriving with the help of my integrative healthcare team.
From Survival to Advocacy
Since then, Dr. Louie’s team has advanced a capsule-based “poop pill”, a non-invasive alternative that’s making FMT more accessible worldwide.
FMT isn’t just for C. difficile—it’s now being researched for:
| Condition | Evidence Level | Promising Findings |
|---|---|---|
| IBS | Mixed | Symptom relief seen in some studies |
| IBD (UC/Crohn’s) | Moderate | 30–40% remission in active disease |
| Post-transplant recovery | Early-phase | Effective microbiome restoration |
| Metabolic conditions | Preclinical | Promising early trials |
| Neuropsychiatric conditions | Experimental | Early but hopeful results |
More Than Medicine: A Holistic Approach
At times, the medical system has played an important role in my health—through invasive procedures, IV antibiotics, and ultimately FMT. For that support, I’ll be forever grateful.
But it wasn’t enough to help me fully recover.
The aftermath of chronic fatigue, nutrient depletion, and emotional trauma demanded more. I embraced nutrition, movement, nervous system regulation, and self-advocacy. I refused to be a passive patient. I became someone with agency—and purpose.
Why I Started PHAM
From undiagnosed endometriosis to early-onset menopause to C. diff, I’ve seen firsthand how a healthcare system can silence patients or encourage them to be passive participants in their health. PHAM—the Preventative Health Awareness Movement—exists to share real stories and empower individuals, to become the CEOs of their health.
We deserve healthcare that listens, prevents, personalizes, and empowers.
Final Thoughts
I never expected my son to be my hero, or for healing to come via poop. But sometimes transformation comes wrapped in unexpected packages. Today, I’m grateful—grateful for life, for my voice, for the platform I have created. And my mission is clear:
Tell your story. Advocate and lead yourself. Know your body. Embrace holistic healing.
Your health, your voice, your story—they matter!